Fast Form Creator
EMR TOUR
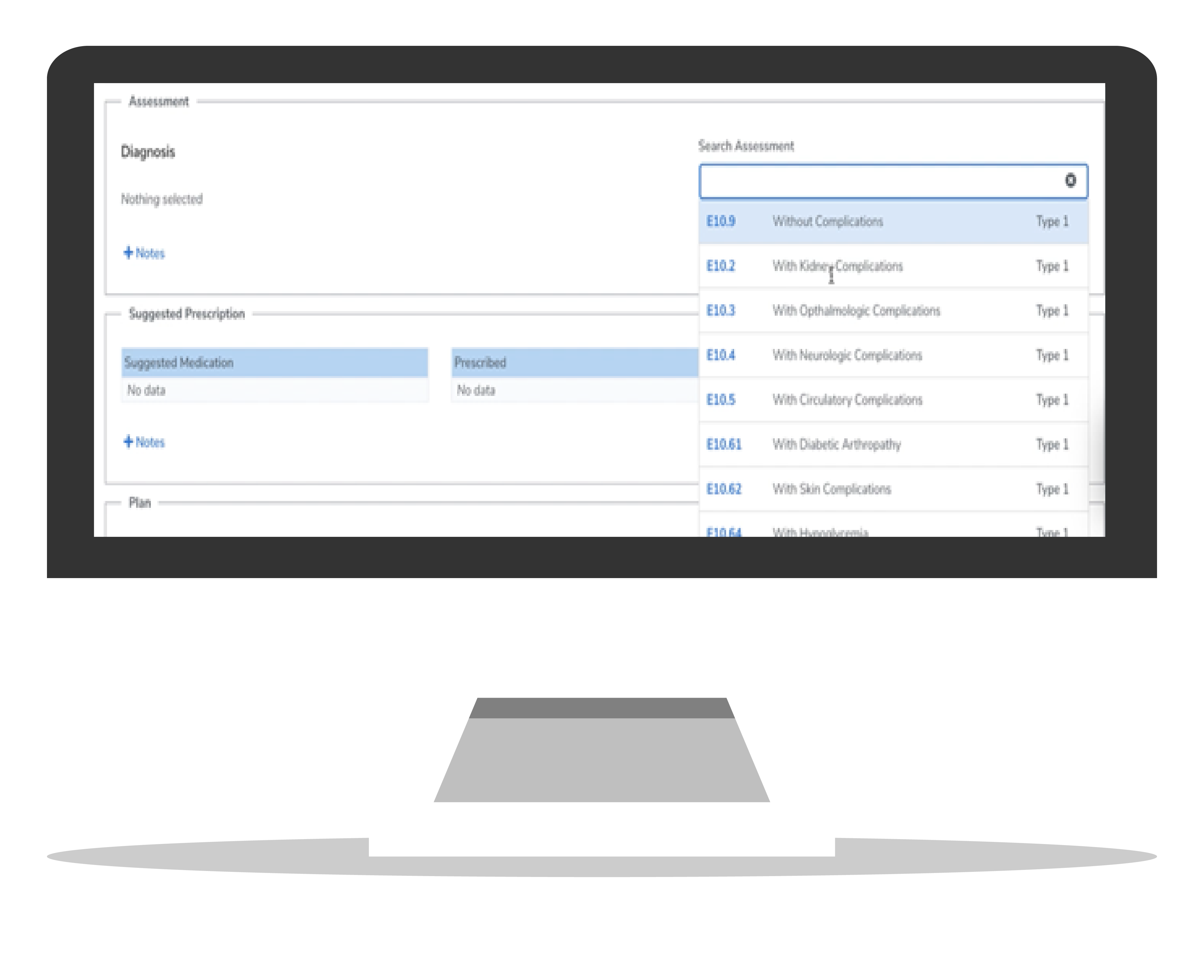
Assessment Tools
ICD 10 & DSM 5
ICD-10 diagnosis is considered invalid if they have not been coded to the full amount of characters required for that code (source: CMS.gov, ICD-10-CM official guidelines for coding and reporting FY 2015). In other words, an incomplete diagnosis is an invalid diagnosis. For this reason, many people use the terms “billable codes” and “valid codes” interchangeably (source: CMS.gov, clarifying questions and answers related to the July 6, 2015 CMS/AMA Joint Announcement and Guidance Regarding ICD-10 Flexibilities).
To help avoid denials or delays in coverage and reimbursements, train your staff to define diagnosis in the greatest detail possible. To support this, CloudMD365 has updated the view of the list of ICD-10 diagnosis, distinguishing the valid diagnosis in black font, and the invalid diagnosis in a lighter, gray font.